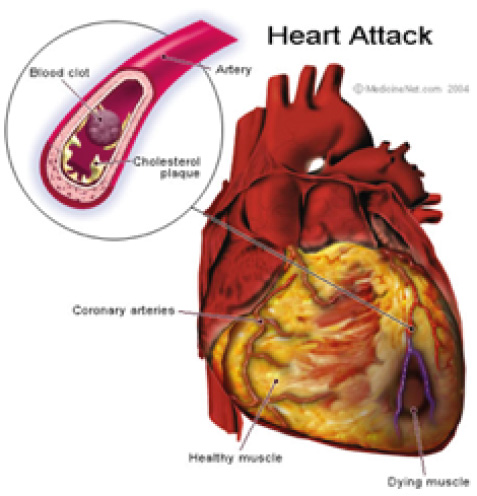
Cord Lining Stem Cells have been used to generate new heart muscle to replace the fibrous tissue from previous myocardial ischaemia to restore it to as-close-to full working pump strength as possible.
Currently, our collaborators, Professor Sonja Schrepfer and Professor Robert Robbins from the University Heart Centre in Hamburg, Germany and Stanford University, USA, respectively are looking at immunological aspects for transplantation of Cord Lining Stem Cells for this application.
Professor Schrepfer’s team has now published two papers characterising the immunological characteristics of Cord Lining Mesenchymal Cells.
The first paper characterises the mechanisms of immunosuppression in Cord Lining Mesenchymal Cells which not only prevent them from being rejected, but also prevent other transplanted cells (like Cord Blood Stem Cells) from being rejected — thus improving their engraftment in the recipient. This paper demonstrates that Cord Lining Mesenchymal Cells appear to be superior to bone marrow mesenchymal stem cells in their immunosuppressant, and thus transplantation, qualities.
Publication: Deuse T, Stubbendorff M, Tang-Quan K, et al. Immunogenicity and immunomodulatory properties of umbilical cord lining mesenchymal cells. Cell Transplantation. 2011; 20: 655-667
The second paper compared Cord Lining Mesenchymal Cells with other mesenchymal stem cells derived from gestational tissue, namely Wharton’s Jelly, placenta and cord blood. It was demonstrated that Cord Lining Mesenchymal Cells were superior to all these other stem cells in terms of proliferation, migration, immunogenicity and immunmodulatory capabilities.
To take a quote from this publication:
“CL-MSCs showed the most promising potential for a cell-based therapy, as the cells showed low immunogenicity, but they also showed enhanced proliferative and migratory potential. Future research should concentrate on the best disease models in which CL-MSCs could be administered.”
Publication: Stubbendorff M, Deuse T, Hua XQ, et al. Immunological properties of extraembryonic human mesenchymal stromal cells derived from gestational tissue. Stem Cells Dev. 2013; (22)19: 1-9
In Professor Screpfer’s own words:
“In addition, these studies show, for the first time, that although immunomodulatory molecules HLA-G, HLA-E, and TGF-β play an important role in MSC immune evasion, intrinsic HLA expression of CL-MSCs seems to be decisive in determining the immunogenicity of MSCs. It is recommended that more research emphasis be placed on CL-MSCs and Cord Lining be the tissue of choice to be saved at birth with Cord Blood.”
Another collaborator, Associate Professor Theodore Kofidis at the National University of Singapore, Is looking at the use of multicellular angiogenic spheroids to improve Cord Lining Stem Cell engraftment in injured heart muscle.
Associate Professor Theodore Kofidis’s team has since published the work described above to show that Cord Lining Mesenchymal Cells embedded in spheroids transplanted onto the heart muscle of mice in cardiac failure reduced the symptoms of cardiac failure and improved cardiac function. This exciting work demonstrates the potential for this to be extrapolated to humans with heart failure in the future.
Publication: Lilyanna S, Martinez EC, Vu TD, et al. Cord lining-mesenchymal stem cells graft supplemented with an omental flap induces myocardial revascularization and ameliorates cardiac dysfunction in a rat model of chronic ischaemic heart failure. Tissue Eng Part A. 2013 Jun; 19(11-12): 1303-1315